In May 2018, the Chief of Naval Operations directed a comprehensive review of Navy Medicine’s ability to support Distributed Maritime Operations and Expeditionary Advanced Basing Operations across all warfighting domains.1 An effective strategy must anticipate the future environment. Although history shows that accurate forecasting is nearly impossible, scenario thinking can help prepare for multiple alternative futures.1, 4, Medical planning for future conflicts is a vital component of support of the National Security Strategy. Using lessons learned from past conflicts and predicting the needs of injured or ill service members are vital for planning. Although attention to conflict in the Pacific appears to be a priority, as it aligns with the national strategy, the Navy and Joint medical leadership must also prepare for various possibilities. Within our discussion, we will use scenario thinking as a framework to identify key questions for analysis.
We will approach our scenario thinking through a four-step process:
- Identifying the driving forces
- Identifying the critical uncertainties
- Development of plausible scenarios
- Discussion of implications and ways forward
Our discussion will focus on Navy Medicine fully understanding the limitations of this approach as the move towards a more joint approach is more effective and realistic. However, this same approach can serve equally effectively in joint discussions. In discussing implications and paths forward, we will utilize a framework of manning, training, and equipping our medical teams.
Identifying the Driving Forces
A common business approach to understanding the driving forces in a changing environment surveys political, economic, sociocultural, technological, legal and environmental (PESTLE) factors.5 It also applies to military healthcare and specifically to combat casualty care. Identification of legal and environmental forces is likely beyond the scope of this discussion, and as such will proceed with a PEST analysis.
Political: The National Security Strategy orients politics for military leaders in developing approaches for potential future conflict. Although this provides the framework, many factors influence the direction of leadership as contingencies and plans are made. The major focus revolves around the complex relationship with China and the potential conflict with Russia. Additionally, there is always the threat of terrorism, non-state actors, the impact of pandemic diseases, cyber threats and other concerns. All these issues will frame strategy and medical planning, as will the formation of the Defense Health Agency (DHA) and the implications for individual services’ medical services. The issues of joint medical forces operating in environments that are not native to the service can potentially cause points of friction if DHA sees this as an imperative.
Economic: Although financial solvency is not typically discussed within the military healthcare framework, discussions regarding supply chain, procurement, and sustainment costs at military treatment facilities and Veterans Affairs healthcare facilities is a significant burden. Procuring medical materials, drugs, and technology in potentially austere environments will be a significant logistics evolution. Supply will be directly impacted by supply chain issues for products produced outside the United States. Demand for new maritime platforms to support the medical mission will need to be addressed and budgeted.
Sociocultural Issues: These can have an impact depending upon the area of operation in which medical care is being provided. Understanding cultural norms for land-based operations will be essential. Additionally, within the Navy medical community, it may be necessary to broaden one’s job description and skillset. Understanding how that will be socialized within the Navy will be vital to providing individuals with the appropriate support for optimal patient outcomes. Recruitment and retention of highly skilled service members is an ongoing issue in our all-volunteer military. Competition with civilian positions, especially within the medical corps, will need to be addressed in some meaningful way.
Technology: Improvements in medical technology, artificial intelligence, and machine learning will have a deep impact in allowing us to address far-forward resuscitative and surgical care. Improvements in blood banking technology and the advent of shelf-storable blood substitutes will probably have the biggest impact on providing resuscitative care close to the point of injury. Cybersecurity will be a limiting factor in utilizing advanced technology for medical care. Mitigation strategies will be necessary for both cybersecurity and, in the situation where communication is lost, for sustainability of ongoing patient care. Demand for technological development will originate from the requirements incurred by operating from atypical platforms and environments requiring advanced medical care. The other impact of technology would include the evolution of new weaponry with effects still to be understood.
Critical Uncertainties
Many variables can influence the direction of combat casualty care for the next conflict. Over the past twenty years, the U.S. military has provided state-of-the-art trauma care in a land-based conflict, resulting in the development of a highly functioning trauma system. The mandate from the Secretary of Defense requiring access to surgical care within 60 minutes (the Golden Hour) nurtured an environment requiring high numbers of tactically distributed medical providers and the necessary support to achieve this benchmark. The patient outcomes demonstrate the effectiveness in which there was an unprecedented 94 percent survival rate if a wounded service member made it to surgical care within an hour of injury. Limiting the U.S. strategy to similar scenarios would be shortsighted. The top two trends that would likely have the biggest impact would be location of conflict (land vs. sea-based) and illness type (trauma vs non-trauma). Graphically, this might be represented as follows:
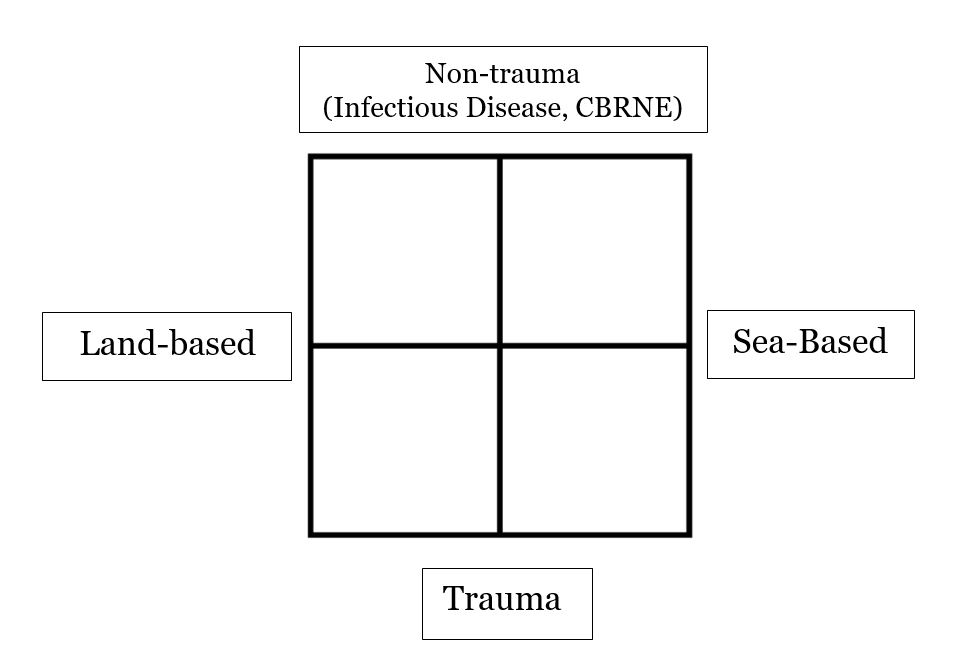
Non-Trauma illness would include all pathologies that would not require initial surgical care as a life-saving measure. This could include infectious diseases, including pandemics, chemical and radiation exposures, and other illness that would impact the war-fighting effort. Trauma, including burns, are injuries caused by kinetic activity. Beyond the current thinking this would include injury caused by new weaponry including directed energy weapons and other advanced technologies. As for location, a sea-based conflict would be burdened by time and space, what is now termed distributed maritime operations. In these situations, there may be access to land-based resources but these may be limited by control of sea lanes and cooperation from foreign governments. As one moves from one quadrant to the next, the demands for medical care can change drastically. It will be necessary in the future to incorporate non-traditional approaches to providing medical care while maintain the highest standards for quality. This will require leaders to think strategically and outside-the-box to develop solutions for complex patient care and environmental issues.
Plausible Scenarios
Land-Based/Non-trauma: The illness complex in this scenario is potentially vast and has the potential to deal with illnesses that we know little or nothing about. A pandemic or other highly communicative disease intersecting with a land-based war would be challenging. In highly contagious diseases, the transmission rate could produce hundreds of patients in a short time. Additionally, if this is an unknown pathogen issue related to treatments and protection of healthcare providers is amplified. High patient volumes would preclude evacuation and would require prolonged care at the epicenter of the outbreak.
Similarly, in a chemical or radiation event, issues related to healthcare provider access and evacuation concerns would be paramount. In any disease state that would require critical care treatments, including mechanical ventilation, continuous infusion medications, or organ support technology (i.e., dialysis), equipment and supply issues would pose a logistics concern. Finally, ethical decisions regarding withholding care would be required to do the greatest good for the greatest number.
Land-Based/Trauma: This scenario is the most familiar to healthcare providers and leaders, as this represents a situation we have effectively dealt with over the past two decades in Afghanistan and Iraq. In that conflict, Navy Medicine was able to participate in a highly functional joint services trauma system that resembles CONUS civilian trauma system. Patient care was driven by evidence-based medicine, outcomes were tracked, and performance improvement was incorporated. The variable that permitted such a highly functioning system was air superiority. What if there was no control of the air? How would our approach to similar injuries differ? Evacuation times would be prolonged, and demands for prolonged care would be required at both role-2 and 3 facilities. The resupply of materials, including medications and blood, would be challenging. Specialized care, typically provided CONUS during the last conflict, would not be readily available because of extended evacuation times.
Sea-Based/Non-trauma: In a sea-based scenario, the issues of space and time become major influences in decision-making. Furthermore, if the disease process originates on a naval vessel, all levels of care are determined by the type of vessel and the organic medical capabilities. In the case of a carrier, the medical resources are limited for the population it serves. Although the carrier strike group has a more robust capability, evacuating critically ill patients may not be possible. In fact, evacuation may not be wise, as this may spread the disease across vessels. If the United States and its Allies are not in control of the sea lanes, then evacuation becomes even more complicated. The issues of patient volume, equipment, and ethics, as in the land-based scenario, are mirrored here but become complicated by time/space and control of the air and sea.
Sea-Based/Trauma: The U.S. Navy has not had to confront sustained mass casualties at sea since WWII. The complexity of dealing with a large volume of severely injured patients in a maritime setting is unique and amplified by the issues of time and distance. Shipboard capabilities vary by platform, and medical expertise may be limited or nonexistent. The challenges of limited supply, medications, and blood further complicate the care of the injured. The organic medical capabilities of the ship may be destroyed by the attack. The damage to the ship will influence holding and evacuation capabilities. Finally, control of sea line and air will greatly influence the delivery of care and the evacuation of the injured.
Implications and Paths
On review of the possible scenarios, several unifying themes start to emerge to address some of the current limitations for the United States. The recommendations allow leaders and front-line workers to consider the way forward for innovation. First, if one considers the issues of the inability to evacuate patients several nodes can be addressed to impact both. The U.S. military medical community needs to utilize providers, beyond physicians, outside their usual job descriptions. This would allow force multiplication to impact many patients in a wide geographic space. The magnitude and effectiveness of enlisted personnel provide a powerful, often under-utilized, workforce that would allow for the delivery of time sensitive, lifesaving interventions in a dispersed environment.
This can only be possible by leveraging technology to improve patient care. Technological innovation can address many of the areas of concern in this discussion. Specifically, telehealth capabilities need to be expanded and applied across the continuum of patient care. Integral to the exploitation of telehealth is to assure adequate cyber security. Although technology may allow the force multiplication is a dispersed environment, consideration for the potential negative effects must be considered. Issues related to the technology itself, such as latency or disconnect must be considered; and the potential issues with the end users, such as failure to recognize complications or the inability to continually monitor a patient following intervention. Some of these negative effects may be mitigated by investment in innovative diagnostic and therapeutic modalities will permit far-forward advanced patient care. These innovations must include artificial intelligence and machine learning to assist caregivers with diagnoses and decision-making. To address issues of resupply, investment in unmanned vehicles, both land, and sea-based, for the specific purpose of resupply and equipment delivery needs to be made. Exploring more capabilities of 3-D and advanced printing can also address some of the resupply concerns.
The issue of prolonged field care touches on all four quadrants of our scenario. Again, leveraging technology for telehealth, innovation in diagnostics and therapeutics, and artificial intelligence to assist caregivers are vital in assuring optimal outcomes. Congruently, novel ideas for patient transport will need to be addressed. New concepts of maritime-based vehicles allowing for transport while advanced and critical care is provided to patients will be necessary. Medically, we will need to explore ideas of “suspended animation” to allow time to be effectively slowed for the patient thereby mitigating the effects of delayed access to specialty care.
Finally, all the scenarios presented pose ethical concerns if we use the experience from our last conflict as our benchmark. For the past two decades, we achieved an unparalleled survival rate. This success may not be achieved in our next conflict. As such, we believe it will be necessary to address the ethics of these potential scenarios. We will need thought leaders to address concerns and provide guidance in limiting medical care. We will need to understand the “breakpoint” between patient salvage and provider safety and redefine the concepts of futility with large-scale illness or injury.
Conclusion
Navy Medicine is likely to face numerous challenges in future conflicts. The framework provided here should enable further discussion of planning for medical care for future conflicts beyond that of a near peer confrontation in the USINDOPACOM area of operations. Although many of the unifying features of all the scenarios are applicable to this focus, more opportunities arise from the discussion of non-trauma scenarios and conflicts without control of the air or sea. Benefits of exploring in this way include addressing potential blind spots by listening to and incorporating critical thinking and input from expertise outside medicine (engineering, economics, education, industrial psychology); this will be the necessary for the successful response of Navy Medicine and Joint Medical Forces to future conflicts.
Originally published in Center for International Maritime Security (CIMSEC): https://cimsec.org/scenario-thinking-for-combat-casualty-care/
Authors’ note: This article resulted from a group project for Naval Postgraduate School course GB3400: Critical Thinking for Strategic Leadership. The course is centered on students developing their critical and strategic thinking skills, and to better understand how to use critical thinking as a tool for strategic leadership in and of organizations and its importance for national security.
Commander (Dr.) Art Valeri is an Operative Dentist stationed at NMRTC Great Lakes serving as the Department Head/Chief, Dental Service of the Veterans and Military Staff Hospital Dental Clinic, Captain James A. Lovell Federal Health Care Center, North Chicago, IL.
Commander (Dr.) Jay Yelon is a US Navy Trauma Surgeon stationed at the Military-Civilian Partnership at the University of Pennsylvania. He is a Professor of Surgery at the Uniformed Services University of Health Sciences, F. Edward Hebert School of Medicine.
Lieutenant Commander Juanita Hopkins is Registered Nurse and resident student at the Naval Postgraduate School, Monterey, California.
Lieutenant Seamus Markey is a US Navy Human Resources Officer serving as the Human Performance Program Officer at Recruit Training Command, Great Lakes, IL.
References
1. Gillingham B, Dagher K. Letter in response to Joint Integrative Solutions for Combat Casualty Care in a Pacific War at Sea. JFQ 96, 1st Quarter; 2020.
2. National Defense Strategy 2022. defense.gov. Accessed September 14, 2022.
3. Kahn H. In Defense of Thinking. https://www.hudson.org/national-security-defense/in-defense-of-thinking. 2020.
4. Augier M, Barrett S. Cultivating Critical and Strategic Thinkers. Marine Corps Gazette. July 2019.
5. Walsh K, Bhagavatheeswaran L, Roma E. E-learning in healthcare professional education: an analysis of political, economic, social, technological, legal and environmental (PESTLE) factors. MedEdPublish; 2018, p 97.
Featured Image: PHILLIPINE SEA (April 20, 2022) Hospital Corpsman 2nd Class Anthony Castro, from Kissimmee, Fla., assigned to amphibious transport dock ship USS John P. Murtha (LPD 26) stabilizes the head and neck of a simulated casualty during a Mass Casualty Drill. (U.S. Navy photo by Mass Communication Specialist 2nd Class Curtis D. Spencer)

